Introduction to Multimorbidity and Nutrition
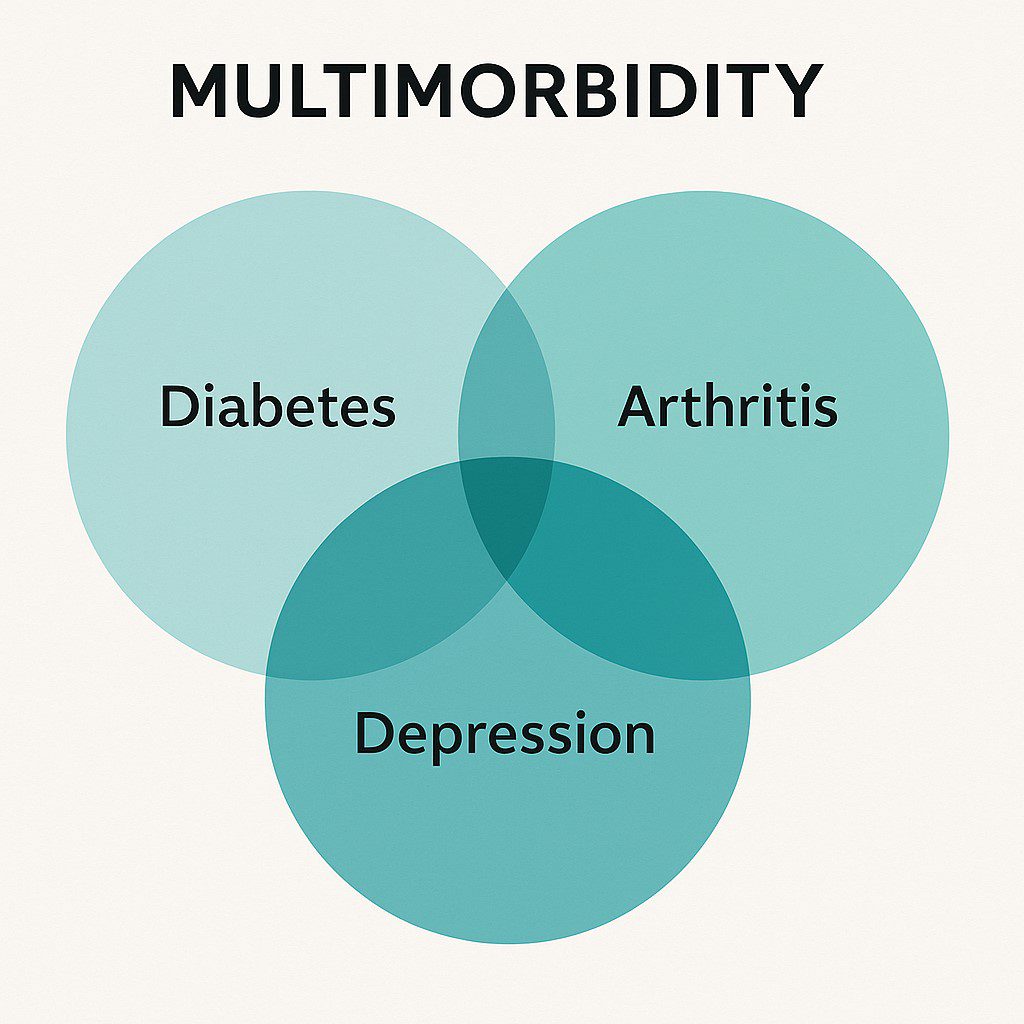
Multimorbidity—the coexistence of two or more chronic diseases such as type 2 diabetes, cardiovascular disease, arthritis, and depression—is a growing global health challenge. Traditional medical care often addresses each disease separately, missing the interconnected biological roots like systemic inflammation and metabolic dysfunction. Emerging research highlights a paradigm shift: nutrition is no longer supportive but therapeutic. It influences disease progression, symptom management, and quality of life across multiple conditions.
The Biological Basis of Multimorbidity.
Many chronic illnesses share common pathways:
-
Chronic low-grade inflammation
-
Oxidative stress
-
Insulin resistance
-
Dysregulated immune response
For example, pro-inflammatory diets high in sugar and processed foods can worsen both heart disease and depression. In contrast, anti-inflammatory diets rich in whole foods, omega-3s, and antioxidants can help modulate these root causes.
Personalized Nutrition and Functional Medicine Approach.
Moving beyond generic dietary advice, personalized nutrition tailors interventions based on genetics, microbiome health, lifestyle, and food sensitivities to manage chronic diseases. Functional medicine uses this information to:
-
Identify root causes of disease
-
Design targeted elimination diets
-
Use food-as-medicine strategies
-
Incorporate individualized supplementation
This approach helps create sustainable, long-term dietary change for better outcomes.

Dietary Patterns and Their Impact.
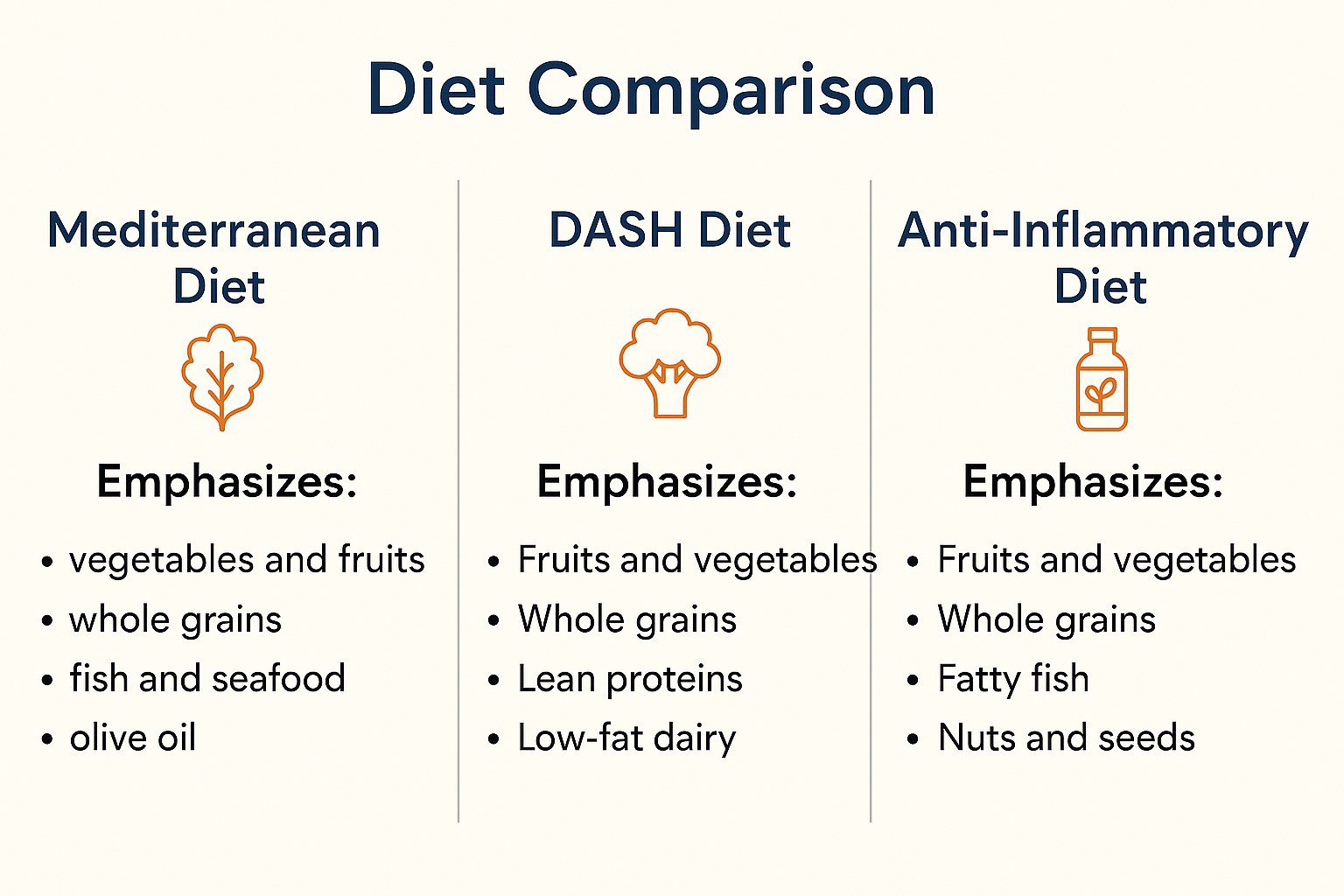
Certain evidence-based diets stand out in managing multimorbidity:
-
Mediterranean Diet: Heart-healthy, anti-inflammatory, and glycemic-control-friendly.
-
DASH Diet: Reduces hypertension and improves metabolic health.
-
Anti-inflammatory Diets: Reduce processed foods, emphasize antioxidants and plant foods.
-
Plant-forward Diets: Boost gut health, lower cholesterol, and improve insulin sensitivity.
Each of these can be adapted based on cultural and personal preferences, improving both compliance and effectiveness.
Nutrients That Matter
Specific nutrients play critical roles in reversing or managing chronic disease mechanisms:
-
Magnesium – Regulates blood pressure and insulin function
-
Vitamin D – Balances immune and inflammatory responses
-
Omega-3 Fatty Acids – Supports cardiovascular and mental health
-
Polyphenols – Antioxidants found in berries, green tea, dark chocolate
-
Fiber – Reduces inflammation and improves gut health
Deficiencies in these nutrients are common in chronic illness and must be addressed through diet or supplements.
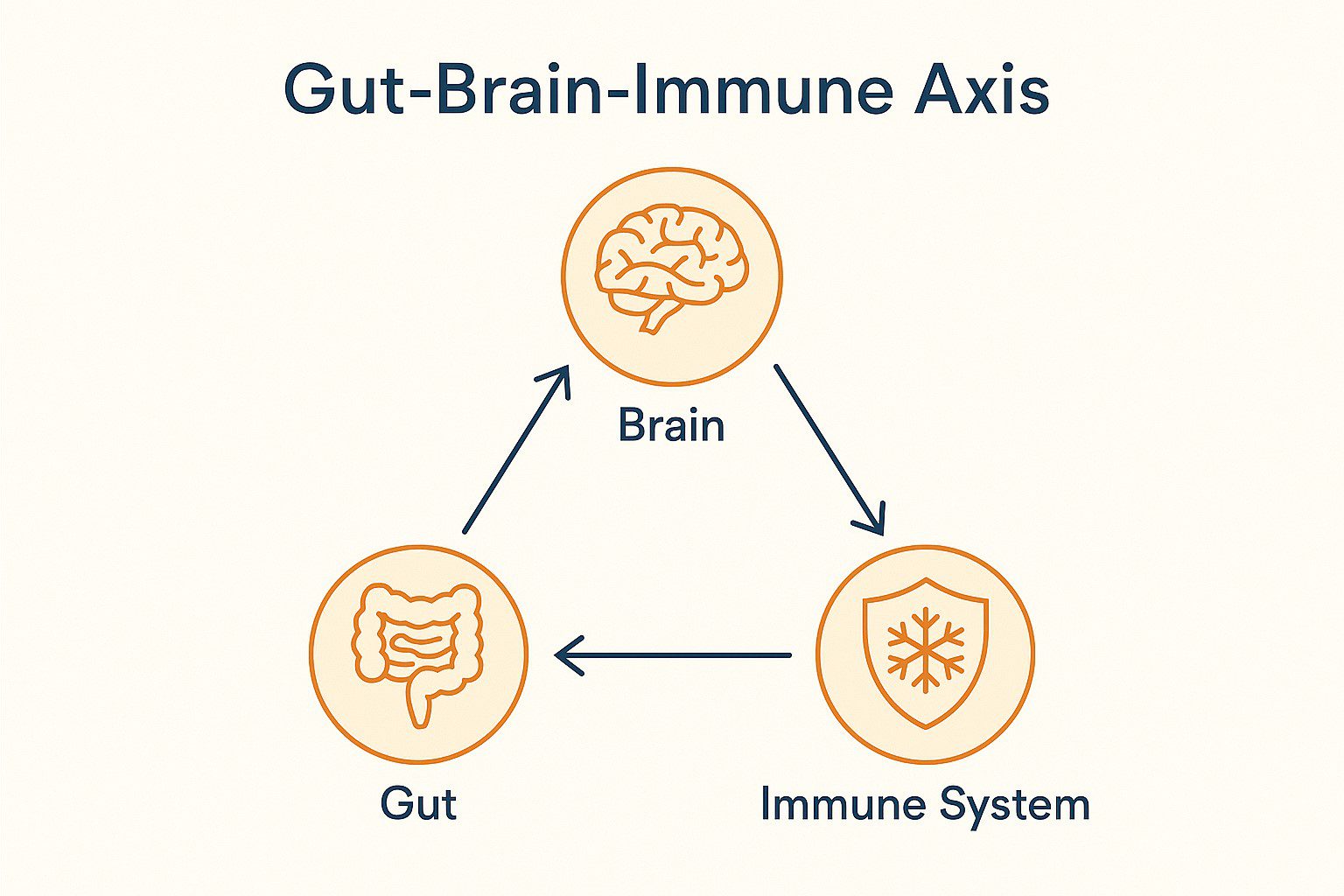
Role of the Gut Microbiome.
The gut microbiome influences everything from immune regulation to mental health. Dysbiosis—an imbalance in gut bacteria—is linked to conditions such as:
-
IBS
-
Obesity
-
Autoimmune disorders
-
Depression
To support microbiome diversity:
-
Eat fiber-rich foods
-
Incorporate prebiotics (onions, garlic, bananas)
-
Add probiotics (yogurt, kefir, fermented vegetables)
Emerging science suggests gut health improvements can enhance outcomes across many chronic conditions.
Practical Implementation Strategies.
Effective implementation of nutrition-based care requires coordination between doctors, nutritionists, and patients. Key strategies include:
-
Conducting dietary assessments
-
Offering behavioral counseling for sustainable change
-
Developing meal plans and shopping guides
-
Providing ongoing monitoring with biomarkers and follow-ups
-
Enhancing nutrition literacy for self-management

Barriers and Challenges Despite the growing evidence.
Despite the evidence, many barriers remain:
-
Limited time and training in clinical nutrition
-
Socioeconomic constraints and food access
-
Cultural dietary preferences
-
Patient adherence and motivation
Solving these requires a systems-level approach, policy changes, and integrative care models that include nutrition as a core service.
Case Study Example Patient:
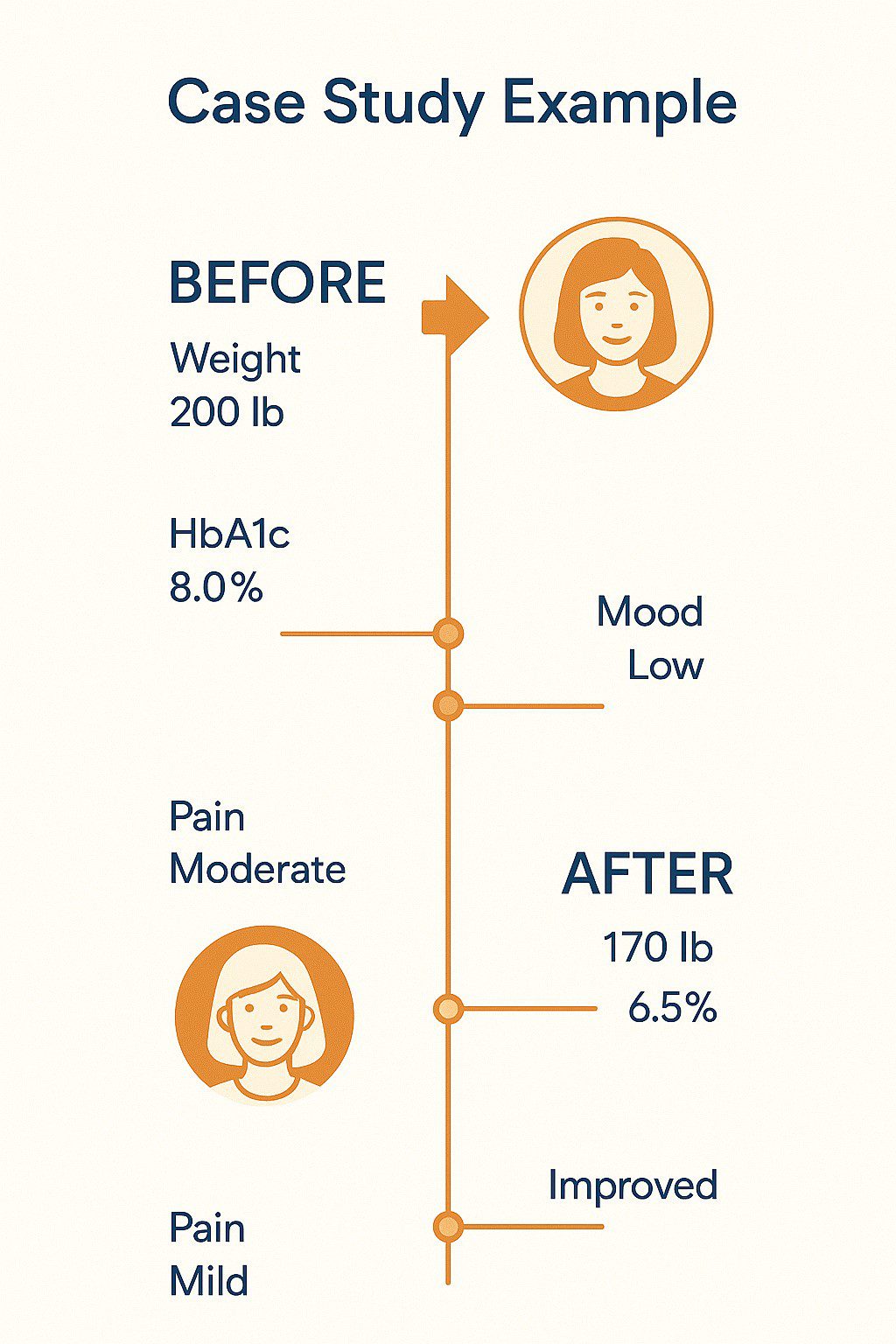
Patient Profile: 55-year-old woman with type 2 diabetes, obesity, osteoarthritis, and depression.
Intervention:
-
Transitioned to a Mediterranean-style anti-inflammatory diet
-
Provided weekly meal planning and grocery support
-
Supplemented with vitamin D, omega-3s, and magnesium
-
Collaborated with both a nutritionist and primary care physician
Outcome After 12 Months:
-
10 kg weight loss
-
Improved HbA1c and glycemic control
-
Reduced joint pain
-
Improved mood and energy levels
Conclusion and Future Directions.
The future of multimorbidity management lies in:
-
AI-driven personalized nutrition plans
-
Microbiome-informed interventions
-
Nutrigenomics (diet and gene interaction)
-
Policy-driven public health nutrition programs
Nutrition must become a core pillar of chronic disease care—not a supplement to it. Empowering patients with knowledge and tools to take control of their diets could revolutionize the way we manage chronic illness.
Final Thoughts
As the burden of chronic disease rises, nutrition must evolve from passive support to active therapy. A personalized, root-cause approach can significantly improve outcomes, reduce healthcare costs, and enhance quality of life. The integration of clinical nutrition into routine care is not just innovative—it’s essential.
✅ Take the First Step Toward Better Health
If you or a loved one is managing multiple chronic conditions, it’s time to go beyond symptom control and address the root causes with expert guidance.
👉 Book a Nutrition & Lifestyle Consultation Today
Let our integrative team at Recoup Health support you with a personalized plan tailored to your needs.
🌐 Visit www.recoup.health »
📞 Call Us for Expert Guidance
Have questions or need help booking an appointment?
📱 Call us at: 080-69274900




